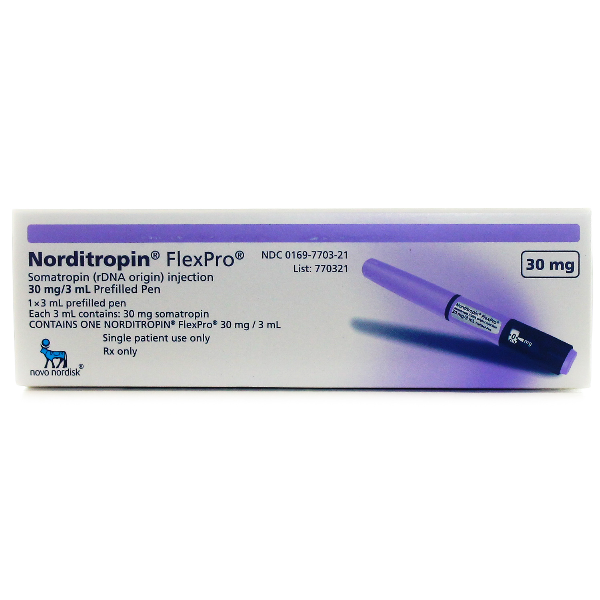
Norditropin
$200.00 – $1,900.00Price range: $200.00 through $1,900.00
Generic Name: Somatropin Injection
Brand Name: Norditropin
Drug Class: Growth Hormone Analogs
About Norditropin Injection
Somatropin, or rh-GH, is a pure form of recombinant growth hormone produced by either mammalian or Escherichia coli bacteria. The pituitary produces endogenous human growth hormone (hGH). In 1956, the first growth hormone was extracted, and its structure was discovered in 1972. Growth hormone (GH) was previously generated from human cadavers prior to 1985; however, this practice was discontinued due to Creutzfeldt-Jakob virus contamination of the product. Somatropin is licensed for use in adults with short bowel syndrome, growth hormone deficit (GHD), growth failure, or short stature, as well as cachexia and AIDS wasting. In studies for the treatment of HIV-associated adipose redistribution syndrome (HARS), somatropin has been shown to reduce visceral adipose tissue, according to limited short-term evidence. There are numerous somatropin medications available, each with unique indications and dose guidelines. It is important to choose products carefully because they could not be interchangeable. The FDA initially authorized somatropin in 1987.
Children and adolescents’ normal skeletal, connective tissue, muscle, and organ growth is stimulated by endogenous growth hormone. Additionally, it’s crucial for adult metabolism. Recombinant goods imitate each of these behaviors. Growth hormone (GH) receptors are occupied by somatropin, which binds to them and causes a variety of direct and indirect physiological consequences. The direct effects include inhibition of insulin’s peripheral action, which in turn stimulates insulin secretion; stimulation of the liver’s and other tissues’ production of somatomedins or insulin-like growth factors (IGFs); stimulation of adipose tissue’s triglyceride hydrolysis; stimulation of the liver’s output of glucose; induction of a favorable calcium balance; and retention of sodium and potassium. These effects, which insulin opposes on the metabolism of fat and carbohydrates, are amplified by glucocorticoids.
The anabolic and growth-promoting actions of somatropin are indirectly mediated by somatomedins or insulin-like growth factors (IGFs). IGFs float around the body and attach to particular IGF receptors. IGF-1 and IGF-2 are the two known IGFs. Growth hormone appears to be primarily mediated by IGF-1, whereas IGF-2 has more insulin-like activity. The main anabolic effects of IGFs include inducing cell proliferation and growth, stimulating amino acid transport, and stimulating DNA, RNA, and protein synthesis. IGF-1 is directly in charge of chondrogenesis, skeletal development, and soft tissue expansion. By altering the cartilaginous growth regions of long bones, linear growth is encouraged. The quantity and size of skeletal muscle cells, the size of organs, and the activation of erythropoietin all contribute to the stimulation of growth. Growth hormones can affect the gut directly or indirectly through the local or systemic synthesis of IGF. Growth hormone has been found to improve the transmucosal transfer of nutrients, electrolytes, and water in in-vivo experiments. Glucocorticoids prevent these collateral effects.
The FDA informed medical experts that it had evaluated SAGhE (Sante Adulte GH Enfant) trial data in August 2011. (a long-term epidemiological study conducted in France). Compared to the general population, individuals treated with somatropin as children with idiopathic growth hormone insufficiency and idiopathic or gestational low stature had a 30% higher risk of death, according to the SAGhe Study. Recombinant human growth hormone with an elevated risk of death: The FDA found this evidence to be inconclusive. [3] An enhanced mortality model was developed in 2016 utilizing the Swedish Medical Birth Registry to calculate the standard mortality rates for growth hormone-treated patients in comparison to the general population. The authors came to the conclusion that, rather than being caused by the administration of growth hormone therapy itself, the rise in mortality observed in the SAGhE study was likely related to fundamental traits of the population affected by growth hormone deficiency (such as birth weight, birth length, and congenital malformations).[4]
Some laboratory results may vary as a result of somatropin medication. With somatropin medication, serum levels of inorganic phosphorus, alkaline phosphatase, and parathyroid hormone may rise.
Patients with a known hypersensitivity to somatropin or any of the product excipients should not take somatropin products. With the usage of somatropin drugs beyond their first release, severe systemic hypersensitivity responses, including anaphylactic reactions and angioedema, have been documented. Patients and caregivers should be made aware that major hypersensitivity responses or anaphylaxis are possible, and that if this happens, quick medical help should be sought.[5][6][1][2][7][8][9][10][11][12] Any hormonal product has the potential to cause a local or systemic allergic reaction. M-cresol is a preservative that is present in a number of the items. In patients with m-cresol hypersensitivity, some formulations advise using sterile water for injection as a diluent; other brands advise using different formulations. When taking somatropin in patients with m-cresol hypersensitivity, the package insert of the individual drug should be consulted for more details. In a similar vein, glycerin is also present in several of the formulas. Glycerin-containing somatropin formulations shouldn’t be used in people who have glycerin hypersensitivity.
Somatropin is contraindicated for promoting growth in children who have epiphyseal closure. These patients are no longer capable of linear growth. In addition, people with endocrine abnormalities or those going through rapid growth may experience slipping capital femoral epiphysis more frequently.
Children’s response to somatropin medication tends to deteriorate over time. However, compliance as well as other causes of growth failure such as thyroid problems, malnutrition, advanced bone age, and antibodies to somatropin should be evaluated in children whose growth rate is not enhanced, particularly during the first year of treatment. A clinician should examine any youngster using somatropin who complains of hip or knee pain or who develops a limp. Patients with endocrine issues or growing youngsters may experience slipped capital femoral epiphysis more commonly. Children who experience growth failure due to renal impairment should also be examined for the development of renal osteodystrophy. Children with advanced renal osteodystrophy may develop slipped capital femoral epiphysis or avascular necrosis of the femoral head; x-rays of the hip should be taken prior to starting somatropin medication. Idiopathic growth hormone deficiency and idiopathic or gestational short stature patients treated with somatropin during childhood had a 30% increased risk of death compared to the general population, according to data from the SAGhE (Sante Adulte GH Enfant) study, which the FDA reviewed in August 2011. Recombinant human growth hormone and an elevated risk of death have been linked, but the data isn’t definitive, according to the FDA; a number of flaws in the study’s design have been identified that restrict how well the findings can be understood. The FDA also examined information from the Agency’s Adverse Event Reporting System and the medical literature (AERS). The FDA will continue to investigate this safety concern and anticipates more information from the SAGhE study in the spring of 2012. When fresh information becomes available, the FDA will tell the public. Recombinant human growth hormone should continue to be prescribed and used by medical professionals and patients in accordance with labeling instructions. [3]
In neonates and individuals who have benzyl alcohol hypersensitivity, several multi-dose somatropin preparations that contain benzyl alcohol should be used with caution. In newborns, benzyl alcohol has been linked to poisoning. Sterile water for injection, USP should be used for reconstitution and only one dose should be administered per vial if somatropin is to be administered to newborns or patients who have benzoyl alcohol hypersensitivity.
Somatropin is contraindicated in patients with active neoplastic disease. Any pre-existing neoplastic disease, specifically intracranial lesions (including pituitary tumors) must be inactive, and chemotherapy and radiation therapy complete, prior to beginning somatropin therapy. In childhood cancer survivors who were treated with radiation to the brain/head for their first neoplasm and who developed subsequent growth hormone deficiency and were treated with somatropin, an increased risk of a secondary malignancy has been reported. Intracranial tumors, in particular meningiomas, were the most common of these second neoplasms. It is unknown whether there is any relationship between somatropin replacement therapy and CNS tumor recurrence in adults. Monitor all patients with a history of growth hormone deficiency secondary to an intracranial neoplasm routinely while on somatropin therapy for progression or recurrence of the tumor. Because children with certain rare genetic causes of short stature have an increased risk of developing malignancies, consider the risks and benefits of starting somatropin in these patients. If treatment with somatropin is initiated, these patients should be carefully monitored for development of neoplasms. Monitor patients on somatropin therapy carefully for increased growth, or potential malignant changes, of preexisting nevi. Somatropin therapy should be discontinued if evidence of neoplasia develops.[9]
Somatropin should not be used in individuals with severe critical illnesses brought on by complications from open heart surgery or abdominal surgery, multiple accidental injuries, or acute respiratory failure. Two placebo-controlled clinical trials in adult patients (n=522) with these conditions found that somatropin treatment (5.3–8 mg/day) resulted in a statistically significant increase in mortality (41.9% vs. 19.3%). It has not been determined if it is safe to continue somatropin therapy in individuals getting replacement dosages for medical conditions for which the drug has been licensed. Therefore, the possible benefit of continuing somatropin medication should be balanced against the potential risk in patients with acute critical diseases (see Prader-Willi discussion).
Genotropin and Norditropin’s manufacturers warn that adult patients with obesity taking somatropin for growth hormone insufficiency may be more susceptible to side effects when dosed based on weight (see Dosage). It could be better to use a daily dosage that is not depending on weight. Additionally, there have been cases of mortality associated with somatropin usage in pediatric patients with obesity and Prader-Willi syndrome (see Prader-Willi discussion).
Patients with Prader-Willi syndrome who are extremely obese or have severe respiratory impairment should not take somatropin. Somatotropin is not recommended for the long-term therapy of pediatric patients with genetically proven Prader-Willi syndrome who have growth failure unless they also have a diagnosis of growth hormone insufficiency. Growth hormone use has been linked to mortality in pediatric Prader-Willi syndrome children who had one or more of the risk factors listed below: severe obesity, a history of respiratory failure or sleep apnea, or an unexplained respiratory infection. Patients who are male and have one or more of these risk factors may be at higher risk. Before starting growth hormone therapy, patients with Prader-Willi syndrome should have their upper airways inspected for obstruction. Treatment with growth hormone should be stopped if patients exhibit symptoms of upper airway blockage (including the beginning or worsening of snoring). If sleep apnea is suspected in any Prader-Willi syndrome patient, that patient should also be watched. All Prader-Willi syndrome patients should also maintain healthy weights and be closely watched for any indications of respiratory infections, which should be identified as soon as possible and quickly treated. Additionally, cerebral hypertension may be more common in Prader-Willi syndrome patients.
Patients with diabetes should utilize somatropin with caution. During somatropin therapy, patients with diabetes or glucose intolerance, as well as those who have risk factors for developing these conditions, should be continuously watched. Obesity (including obesity in Prader-Willi syndrome individuals), Turner syndrome, or a family history of type II diabetes are risk factors for glucose intolerance. Patients should be watched for signs of glucose intolerance since somatropin may decrease insulin sensitivity, especially at larger dosages. Chronic somatropin overdose may result in glucose intolerance or acromegaly. When somatropin is started, it may be required to modify the dosage of antidiabetic drugs. Somatropin is not recommended for use in people with diabetic retinopathy because of how it affects blood glucose levels and insulin sensitivity. [5]
Somatropin administration should be cautious for patients with a history of scoliosis. Growth hormone accelerates growth, which might cause scoliosis sufferers to undergo scoliosis progression. Scoliosis progression should be tracked in patients. In addition, people with untreated Turner’s syndrome, Noonan’s syndrome, and Prader-Willi syndrome may exhibit skeletal deformities, such as scoliosis. These anomalies, which could appear with growth hormone therapy, should be known to clinicians.
Patients using somatropin may experience decreased blood cortisol levels and/or the masking of central (secondary) adrenal insufficiency if they have or are at risk for pituitary hormone shortages. Following the start of somatropin therapy, patients receiving glucocorticoid replacement therapy for previously identified adrenal insufficiency might need to increase their maintenance or stress dosages. Patients who have untreated hypothyroidism will also not respond well to somatropin medication. Due to the increased risk of autoimmune thyroid disease in Turner’s syndrome patients, changes in thyroid hormone plasma levels may occur with somatropin therapy. Periodic thyroid function testing should be carried out, and when necessary, thyroid hormone treatment should be started. [2]
It has been shown that somatropin medication can result in elevated intracranial pressure, papilledema, visual abnormalities, headaches, nausea, and/or vomiting. Within the first eight weeks of somatropin medication, symptoms often started to appear. The symptoms of intracranial hypertension went away either when somatropin medication was stopped or after the hormone’s dosage was decreased. When starting somatropin therapy and at intervals thereafter, funduscopic examination is advised. Patients with Prader-Willi syndrome, Turner’s syndrome, and chronic renal insufficiency may be more likely to develop intracranial hypertension.
Somatropin has not been the subject of adequate and controlled research in pregnant women, and it is unclear whether it could have harmful effects on the developing fetus or the reproductive system. Different levels above the typical human dose used in animal research have not been associated with any fetal damage or reduced fertility. Remind women of reproductive age that somatropin usage during pregnancy has not been investigated in humans, therefore it is uncertain how the medicine may affect the fetus. [5][6][1][2][13]
There is no information available on somatropin’s presence in human milk, its effects on breastfed infants, or its impact on milk production. There are no known negative effects on nursing infants when somatropin is administered to the mother, and there is no evidence that somatropin treatment results in decreased milk production or altered milk composition. Think about the advantages of breastfeeding, the chance that your baby may be exposed to drugs, and the possibility that your condition won’t be treated at all or only partially. Healthcare professionals are urged to notify the FDA if a breast-fed baby develops an adverse reaction to a medication taken by the mother. [5][6][1][2][13]
Turner’s syndrome patients should have rigorous otitis media and other ear diseases evaluations while receiving somatropin because these patients have a higher risk of ear or hearing abnormalities. Turner’s syndrome patients should also be constantly watched for cardiovascular diseases such stroke, aortic aneurysms, and hypertension because they are also at risk for developing these ailments.
Although significant numbers of elderly individuals were not included in somatropin clinical investigations, published clinical experience has not revealed any variations in reactions between geriatric and younger adult patients. An older adult should generally be given care when choosing a dose, usually beginning at the low end of the dosing range. Patients who are elderly are more susceptible to the side effects of therapy than patients who are children or younger adults. Practice recommendations state that only patients with clinical signs of adult growth hormone deficit (GHD) and biochemical proof of adult GHD should be given growth hormone/somatropin. [14]
Patients with HIV-associated adipose redistribution syndrome (HARS) have been treated with somatropin (Serostim); somatropin therapy may be less successful in female patients with HARS than in male patients. In clinical trials, visceral adipose tissue reduction in 47 women receiving somatropin was comparable to placebo (VAT). The concurrent use of estrogen (6 patients) or a lower baseline VAT level compared to men may be the causes of the lack of effectiveness. Numerous clinical research have shown that lower VAT levels are related to a diminished response to somatropin.
Patients, especially children, who experience severe, ongoing stomach pain while using somatropin should be checked for pancreatitis. Patients who have a history of pancreatitis or who have risk factors for it should use this medication with caution. Rare reports of pancreatitis in both adults and children receiving somatropin have been made, with pediatric patients appearing to be at higher risk than adults. When receiving somatropin medication, girls with Turner syndrome may have an even higher chance of getting pancreatitis than other patients.[7]
| Dosage | 10 mg, 15 mg, 30 mg |
|---|---|
| Quantity | 2 Pens, 3 Pens, 4 Pens, 5 Pens, 10 Pens |
Be the first to review “Norditropin” Cancel reply
Related products
Steroids
Steroids
Steroids
Steroids
Steroids
Steroids
Steroids
Steroids










Reviews
There are no reviews yet.